Recent discussions by the CDC’s Advisory Committee on Immunization Practices (ACIP) about potentially delaying the hepatitis B vaccine for newborns have brought renewed attention to this serious infection. While ACIP ultimately tabled the proposed delay, the debate underscores the importance of understanding hepatitis B and why early vaccination remains crucial for protecting public health.
Epidemiology and Transmission
The World Health Organization estimates that over 250 million people were living with chronic hepatitis B in 2022, with the infection resulting in nearly 1 million deaths. Before widespread vaccination, hepatitis B was far more prevalent. In the 1980s, an estimated 200,000-300,000 Americans became infected annually, with particularly high rates among young adults. Healthcare workers faced occupational infection rates as high as 1-2% per year. Following the introduction of routine infant vaccination in 1991 and catch-up programs for older children and high-risk adults, annual infections have plummeted to fewer than 20,000 cases, representing one of vaccination’s most dramatic public health success stories.
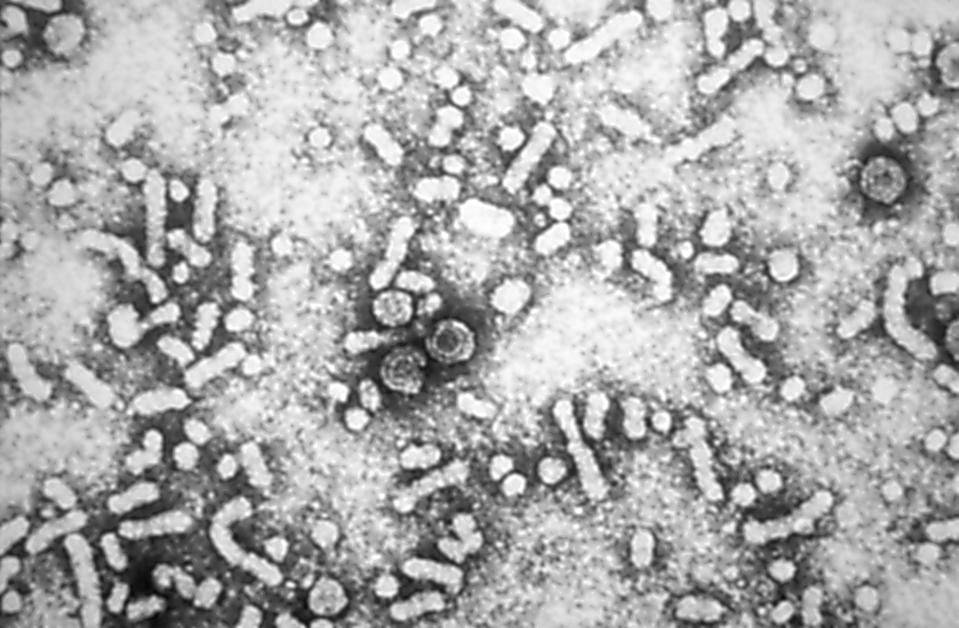
Hepatitis B virus (HBV) is estimated to be 100 times more infectious than HIV and transmits through contact with infected blood and body fluids. Perinatal transmission, occurring when an infected mother passes the virus to their newborn during childbirth, represents the highest risk. Without intervention, up to 90% of infants born to mothers with active hepatitis B infection will become infected.
Sexual contact accounts for the majority of adult infections in the United States, as the virus spreads through unprotected sexual activity with an infected partner. Injection drug use with shared needles or equipment also poses significant transmission risk.
Less common but important routes include exposure to contaminated medical equipment, sharing personal items like razors or toothbrushes with infected individuals, and occupational exposure among healthcare workers. Importantly, hepatitis B does not spread through casual contact, sharing food, or respiratory droplets.
Clinical Manifestations and Disease Progression
Hepatitis B infection presents differently depending on the age at infection and an individual’s immune response. Acute infection may cause fatigue, nausea, abdominal pain, loss of appetite, and jaundice (yellowing of the skin and eyes). However, many people, particularly infants and young children, experience no symptoms initially.
The real danger lies in chronic infection, which develops in up to 90% of infected infants, 30% of children under five, and 5% of adults. Chronic hepatitis B can silently damage the liver for decades, eventually leading to cirrhosis, liver failure, and hepatocellular carcinoma (liver cancer).
Chronic carriers, even when asymptomatic, remain infectious throughout their lives and face a 15-25% lifetime risk of dying from liver disease. This makes prevention through vaccination critical.
The Impact of Hepatitis B Vaccination
The hepatitis B vaccine represents one of modern medicine’s greatest public health achievements. Since routine infant vaccination began in the United States in 1991, new infections have declined by more than 95% among children and adolescents.
Global data demonstrate similar, dramatic results. Countries implementing universal infant vaccination have seen chronic infection rates in children drop from 10-15% to less than 1%. Taiwan, which introduced universal vaccination in 1984, documented a 75% reduction in liver cancer rates among vaccinated cohorts.
The vaccine’s effectiveness extends beyond individual protection. By preventing chronic infections, vaccination breaks the cycle of transmission and provides community-wide benefits.
Why Early Prevention is Critical
The timing of vaccination is extremely important with hepatitis B, since the age at infection is inversely proportional to the risk of developing chronic infection. While adults have only a 5% chance of developing chronic infection, the risk rises to 30% in children under five and approaches 90% in newborns.
Administration of the vaccine at birth delivers multiple benefits. It provides immediate protection against perinatal transmission, offers a safety net for infants whose mothers’ hepatitis B status may be unknown or incorrectly documented, and protects against early childhood exposure from infected household contacts.
Studies from countries that delayed vaccination have documented increased perinatal transmission and subsequent chronic infections. Any gaps in early protection can have lifelong consequences, as chronic hepatitis B remains largely incurable despite available treatments.
Extensive safety data spanning over three decades demonstrate that hepatitis B vaccines have an excellent safety profile. Serious adverse events are extremely rare, occurring in fewer than one in a million doses. The most common side effects include mild soreness at the injection site and low-grade fever, which resolve within days. The benefits of preventing a potentially fatal chronic infection far outweigh the minimal risks associated with vaccination.
Hepatitis B vaccination represents one of public health’s greatest success stories. Reducing the rate of infection early in life has a significant impact on lowering the rates of chronic infection, liver disease and death.